
The ACG System is often used in large-scale, population-level reporting to determine disease risk or prevalence for a specific community, giving population health professionals insights into planning effective strategies and resources.
However, it can also be just as impactful in smaller-scale settings — giving providers access to a wealth of specific patient information which can be tailored to the patient’s immediate needs. Providers can discuss their top medical concerns with the patient while they are in the office. This focus on the individual patient means health issues can be addressed faster, and complications may be avoided.
Today we are sharing the following top 10 reporting metrics providers can access through the ACG System, to determine overall patient health:
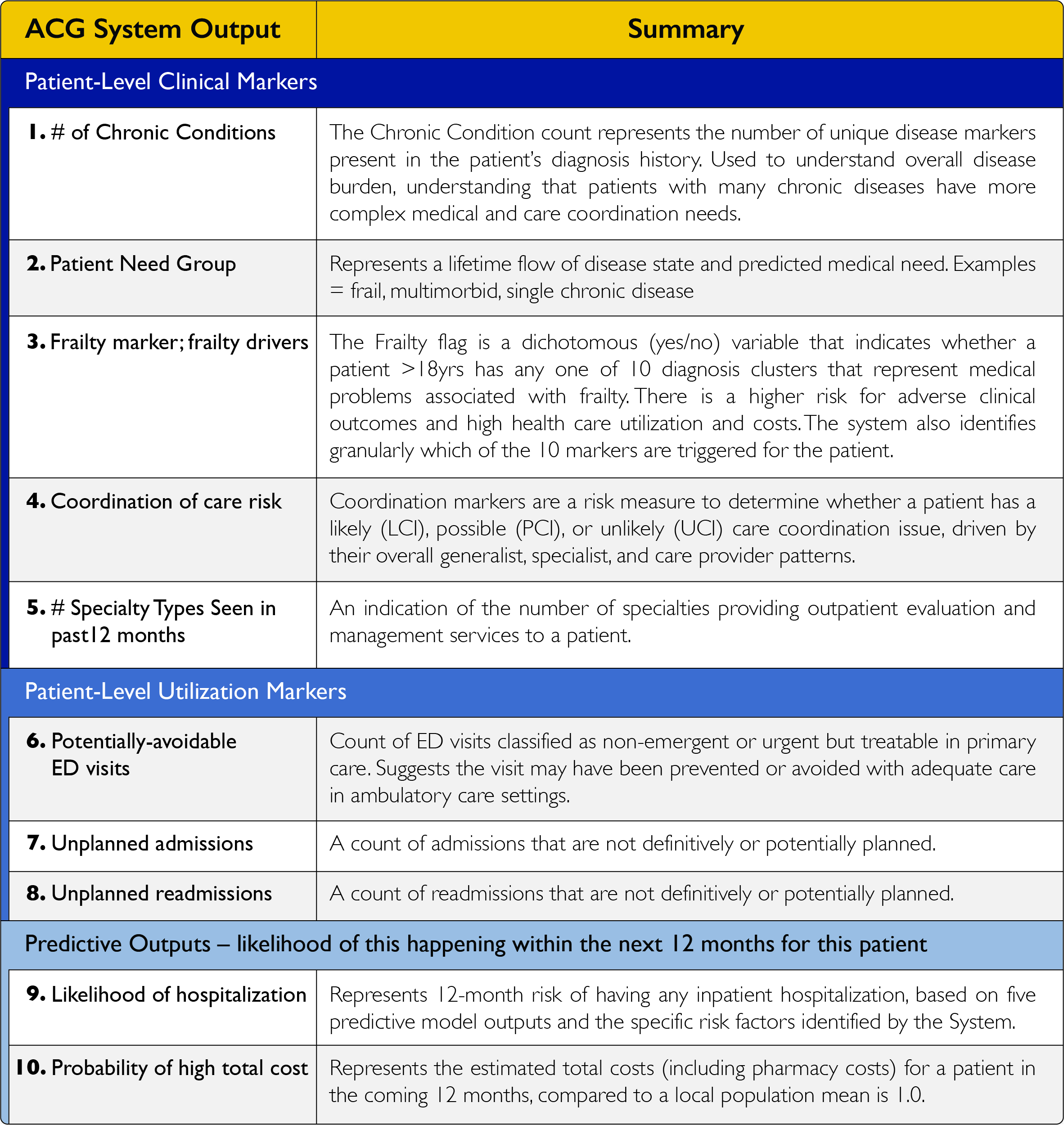
The chart above is divided into three sections: clinical markers, utilization markers and predictive models. Clinical markers provide important insights into factors that can impact a patient’s overall health — such as a chronic condition or care coordination issue. By using these metrics, the provider also learns more about the patient through our Patient Need Group functionality. Patient Need Groups are a high-level segmentation method that identifies patients who are high or rising risk, and pinpoints current and future health care needs.
Another important clinical marker is Frailty. Dementia, fall risk, malnutrition and social support needs can all be observed through this variable. Coordination of care risk includes each of the ways that a patient’s care is managed, including medication, utilization of community resources and communication of the patient’s goals. A total count of specialists seen in the past 12 months further identifies care coordination issues, driven by their overall generalist, specialist and care provider patterns.
Utilization markers include recent avoidable Emergency Department (ED) visits and unplanned admissions or readmissions. Many health concerns can be addressed with a visit to a primary care provider’s office or an urgent care, instead of a trip to the ED. A provider can discuss expectations with the patient should a similar health issue arise in the future. These markers can also give insight into other patient-level issues that affect their ability to receive care.
Predictive models look at future care for an individual. The ACG System features regression-based models that predict the likelihood of an event within the next 12 months, based on a patient’s historical data. A high predictive score for likelihood of hospitalization or high cost can signify a greater chance of a medical episode over the next year. The provider can use this information to prepare the patient and encourage better care to potentially avoid utilization or negative outcome.
Providers require accurate and rapid results when reviewing health-related metrics and reporting. The ACG System offers both large- and small-scale solutions for providers and health systems alike, which allows for better planning and strategy development for individuals and communities, and better 1-1 patient care.
If you have any questions or want to learn more about provider metrics in the ACG System, please email us at acginfo@jh.edu. If you are an existing ACG System customer, please contact your account manager.
Follow Us